Achieving UHC by 2030: What does this mean?

Happy World Health Workers Week! This week the international community has united to show its love for health workers, and a common theme that has emerged this year is the importance of health workers in achieving universal health coverage (UHC). This is particularly relevant given that sustainable development goal (SDG) advocacy is in full-force as the international community works towards finalizing the goals and establishing core indicators to be reached by 2030.
Reaching UHC is imperative to the achievement of SDG 3 – Ensure healthy lives and promote well-being for all at all ages – and its importance is recognized across the global public health community. This is reflected in SDG sub-goal 3.8:
“Achieve universal health coverage (UHC), including financial risk protection, access to quality essential health care services, and access to safe, effective, quality, and affordable essential medicines and vaccines for all.”
But the critical question this sub-goal has raised is “how do we achieve UHC?”
There is no single answer to this question. However, in a 2014 report put forth by the Sustainable Development Solutions Network (SDSN), three key components to an effective UHC system are identified:
- Adequate human resources
- Adequate facilities fully provided with essential equipment and supplies
- Adequate financial resources so everyone can obtain necessary health services without financial hardship
The first, and arguably the core, component to UHC is having adequate human resources. But what does that mean? And more importantly, what does that look like?
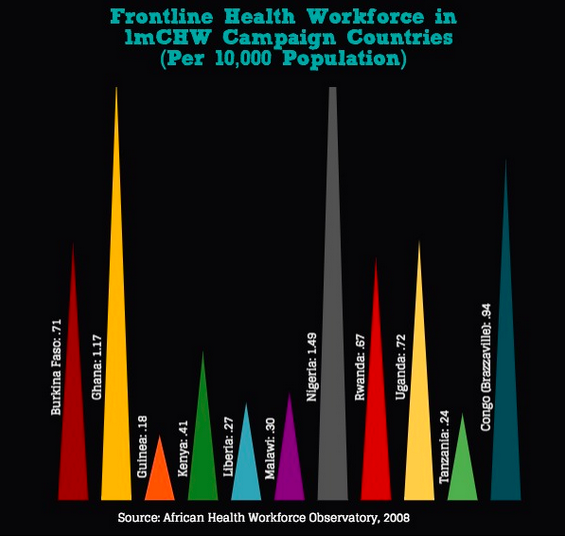
While the SDG indicators for sub-goal 3.8 are still under consideration, the WHO suggests that countries should have at least 2.5 health workers per 1000 people to achieve adequate health care coverage. Although this number is a very rough estimation, it serves as a good basis to compare access to health care across countries. Achieving this level of coverage – which includes access to nurses, midwives, community health workers (CHWs), and other skilled health workers – is not out of reach, especially if we look to strengthening and introducing lower cadres of health workers, such as CHWs, into the formal health sector.
CHWs are a core component of the health workforce, and are increasingly being recognized as such. Because they are members of the communities that they serve, CHWs can ensure that basic primary healthcare services are made available to people everywhere, particularly in rural and low-resource settings. When properly trained, equipped, and deployed at a proper ratio (approximately 1 CHW per 500 people) CHWs can bring diagnostics and treatment to communities who might otherwise go without care. Given their breadth of reach, scaling-up CHWs provides countries, particularly low and middle-income countries, with an opportunity to increase access to health care for their citizens.
So, how do we do this?
To keep it simple, it all comes down to one thing: money. A robust health system costs money. The National Academy of Sciences estimates that, sub-Saharan Africa spends an average of $25 per capita on health care, which is less than half of the $86 per capita spending recommended for achieving UHC. As we’ve seen from the Ebola epidemic, low-income countries do not have the resources necessary to achieve UHC on their own. Making UHC a reality does not only require that we have enough health workers, it rests upon the basic fact that health system strengthening has to be a key priority amongst governments. If governments don’t begin to prioritize health system strengthening and health expenditures, then the international donor community won’t recognize the need to increase funding for this critical need.